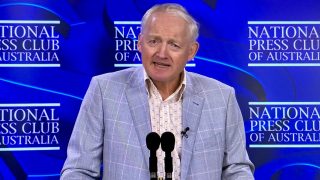
It was a conversation with River City Labs founder and tech entrepreneur Steve Baxter that sparked the idea for Elliot Smith.
Smith, who at the time had just finished a PhD in image-guided radiation therapy and was working as a researcher and academic, was interested in making the medical diagnosis process more effective.
“The more I got into it the more I found out that once you’re at the treatment stage a lot of the legwork is already done,” Smith said. “The best thing we can do is to make sure people are getting diagnoses accurately and early to make technologies a success.”
And then he struck up a conversation with Baxter at River City Labs about friends that had been diagnosed with cancer.
“He was telling me that he was tired of hearing stories from friends where doctors have said, ‘if only we had caught this sooner’, and it all came together,” Smith said.
Smith thought he had a way to stop those conversations from happening and give those with cancer a better chance of recovering using artificial intelligence technology.
A few days later, Baxter called him saying he wanted to support the idea.
Baxter would eventually provide angel funding to Maxwell Plus, Smith’s start-up focusing on diagnostics and technology in health.
After bringing on board chief medical officer Dr Peter Swindle, the company decided that the diagnosis of prostate cancer would be its first focus.
“I spent some time developing the early AI models and finding areas where there was a strong unmet need for this technology, and I landed on prostate cancer,” Smith said.
“It’s very prevalent and, contrary to popular belief, it’s not just old men.”
Maxwell Plus has since been through the River City Labs accelerator program, and closed a $3.4 million funding round led by the CSIRO’s Main Sequence Ventures fund in October 2017.
The company offers a digital clinic which streamlines the assessment and diagnosis of prostate cancer, using artificial intelligence technology tailored to clinicians and patients.
Its web-based platform analyses medical data, including medical imaging, blood and genomic data, to manage the risk of prostate cancer.
It aims to reduce the cost of prostate cancer testing and treatment, and diagnose the disease as early as possible.
“We use AI to analyse all the data that they have and any data that comes in the future through our testing process, and using that we can give them the most accurate screening or diagnosis possible,” Smith said.
“The AI can read more into the data than a physician usually would.”
The platform is designed to be easy to use and as unobtrusive as possible.
“Say you’re a 50-year old man and your employer has promoted this to you as an employment benefit - what would happen is we would collect some demographic information about you to get a first picture of what your risk is, and start on a personalised program,” he said.
“From there you would go and get a PSA test, and that on its own isn’t actually that accurate, but that’s where the AI comes in. We combine that test with those other factors, and any others that come in like MRI scans and genetics.
“All these things come together to give a very personalised and very in-depth picture of your risk of prostate cancer. That will be paired with a clinician who would see the output from the AI, review that and communicate to you through the platform about what your current risk is and what the recommended next step is.”
The Maxwell Plus platform is now in the market in Australia and New Zealand, and the company is currently working through the regulatory process in the US, with plans to launch at the end of this year or early next year.
“It’s a long process and there’s a lot of paperwork involved but if you’re doing the right things and building a quality piece of technology, and employing the high-quality engineering practices, then it’s not that hard,” Smith said.
“You have to make sure you’re doing the right thing and thinking about the clinical outcomes in the proper scientific way, then yes there’s paperwork and costs but it’s certainly not an insurmountable process.”
The start-up is also looking to apply its technology to other medical conditions, and has received a $1.1 million federal government Cooperative Research Centre Projects grant to fund the development and rollout of a similar platform to help with the detection of early-stage Alzheimer’s disease and dementia. Maxwell Plus is working on the project in collaboration with I-MED, CSIRO and Austin Help.
“Our big, hairy, audacious goal is to become the place where you can sign up, and AI and clinicians will together manage the risk of a number of high-risk diseases, and you know that if any diseases were to pop up, you’d know about them far enough in advance to have the best treatment options and for them to stop becoming life-threatening,” Smith said.
While a central concern around artificial intelligence technology is that it will replace humans, leading to job losses and ethical quandaries, Smith said the platform is very focused on AI and doctors working together to produce the best result for the patient.
“We’re still a long way from doctors losing their jobs to AI,” Smith said
“Doctors and AI tend to work best together. The other thing is that if you look across Australia there is probably more demand for the knowledge capability of doctors than we can currently supply, especially in rural settings.
“AI is a great tool to extend the capability of current clinicians to get them there, but it’s a long way from exhausting the supply of clinicians.”
Maxwell Plus is calling on any males aged 40 or above to visit its website to see if the platform would work for them, and to get tested for prostate cancer.