When Dr Tom Kelly started out in medical school, little did he know that he would be building software to diagnose conditions using artificial intelligence.
Back in 2018, while working as an intern at Royal Melbourne Hospital, he became aware of the need for better access to care.
His early experiences working with GPs in rural and regional settings in Horsham and later in Wangaratta drove him even further to investigate.
After seeing lots of patients with missed or delayed diagnoses presenting to doctors and emergency departments, there is one that stands out for the young doctor.
“I saw a stoic, tough farmer who had lost a bit of weight, he presented with vague abdominal pain that ended up being bowel cancer. He'd put off seeing his GP because they'd been booked out for a couple of months.”
Dr Kelly adds that patients like the farmer may have been seen to earlier if they'd had access to technology to triage them and assess the problems.
”That way we could get them to care quicker; making a diagnosis as a doctor is like driving a car from A to B.”
He explains further.
“When you're tired and rushing because you’ve seen hundreds of patients, without the required resources or senior support, you're way more likely to have a car accident.”
“The biggest challenges are the cognitive biases doctors have, compounded by the difficult conditions we face,” he adds.
He said there are scenarios where doctors have to trade off seeing the next very sick person or spending an extra ten minutes with a current patient, exploring rarer possibilities, all while the next patient slowly deteriorates.
These experiences left Dr Kelly with a desire to improve the access patients had to doctors, by providing patients technology to better triage their own symptoms.
First, he had to find the right team to develop the technology.
“It definitely wasn’t easy,” he recalls. “I relied on my instincts to vet their skills. I studied in each domain; design, product, front and backend engineering beforehand. This was critical to get to a basic understanding so I could be confident in bringing the right people.”
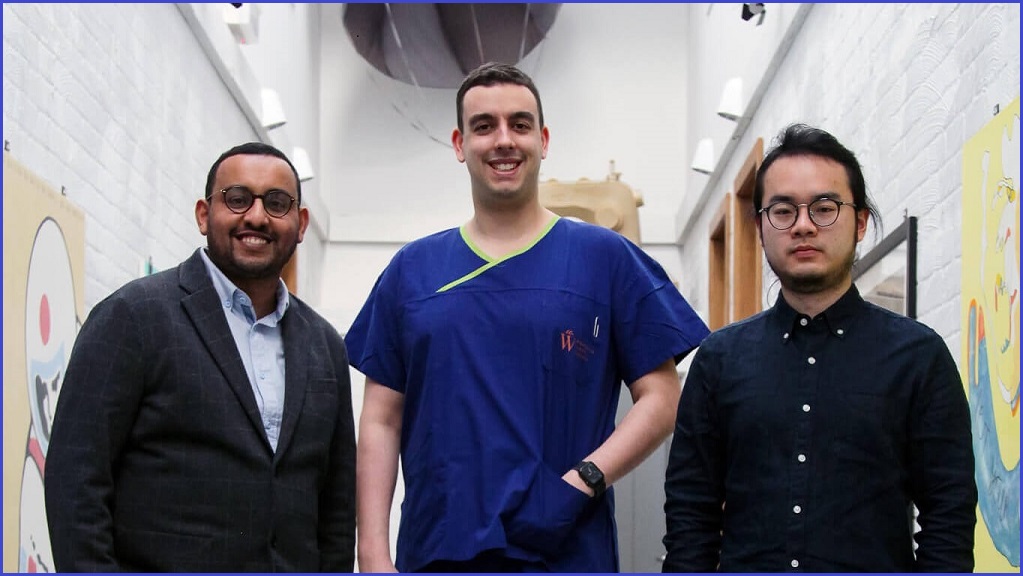
In 2019, he teamed up and founded Oscer with two IT specialists: Waleed Mussa, a strategist with extensive experience in digital transformation who had worked at Goldman Sachs, KPMG and Telstra; and engineer, Yu Liu.
“We all share the same goal of eliminating missed diagnosis; providing easy and safe healthcare,” says Yu Lui.
“We're both technical and can talk in ‘tech’ language, so we always understand each other’s thoughts, even when we have disagreements,” he adds.
Lui’s belief in the idea stems from a personal connection to the problem. He relates to a time he got very ill eating sashimi in Melbourne.
“I felt very weak and could barely get up. But I wasn't sure how serious it was or whether I should call emergency or not. So I tried to find a GP but the earliest appointment was the week after.”
Lui is grateful to a doctor friend who was able to diagnose him over the phone.
“Over the phone diagnosis isn’t easy, but my friend, reassured me with a simple plan of fluids and electrolytes.”
He followed instructions and recovered the next day. “I can’t imagine what I would've done without my friend. Good quality healthcare should be easily accessed by everyone.”
Oscer’s clinical tool is called “Heidi”. Patients enter their reasons to visit their GP including everything from new symptoms, annual health checks and medical certificates.
The program asks a series of questions where patients will describe their symptoms using their voice, free text, photos and multiple choice.
Heidi will triage them to the right visit type: asynchronous chat, voice, video or in-person, then connect patients with their GPs.
“Heidi will get patients from A to B and doctors will review and finalise the consult with the support of our AI. If the farmer I saw had started with Heidi, we would’ve flagged his possible cancer with his GP in hours instead of months.”
Today Oscer is teaching 10,000 medical students how to make better diagnoses with Heidi.
“We're deep in development of our clinical product hoping to get something for patients and GPs by end of 2022,” adds Dr Kelly.
“It's the first tool we've given the world to eliminate missed diagnosis and we can't wait to share our product with patients and doctors.”