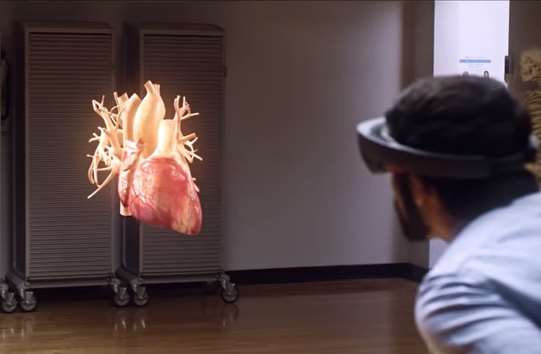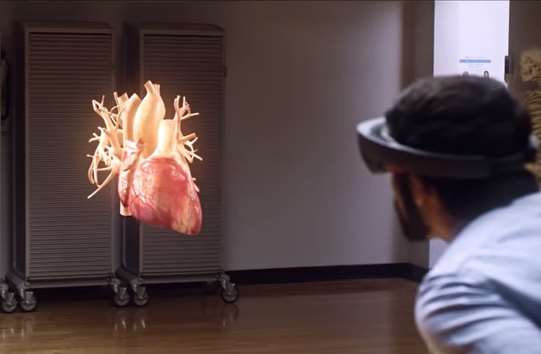
Students use HoloLens to explore cardiac anatomy. (Credit: Microsoft)

Medical schools have started playing with Microsoft’s forthcoming HoloLens augmented reality headset to see what applications it might have in helping train a new generation of health professionals.
Ohio’s Case Western Reserve University is hoping the HoloLens technology will help students better understand the anatomy of the human body – in ways that current methods can’t achieve.
“We’ve been teaching human anatomy the same way for hundreds of years - students get a cadaver, then they look at medical illustrations and it’s completely two dimensional. And the human body isn’t,” Case Western Reserve University president Barbara Snyder said in a video case study.
Professor of radiology Mark Griswold believed the technology could “impact almost everything that we teach people.”
“I think this will improve students’ confidence in learning anatomy dramatically,” he said.
“You can imagine having a class standing around a model [augmented reality skeleton] almost like a tour group in a museum where they’re all interacting completely naturally.”
One of the students lucky enough to have used this application of HoloLens described the way it had helped him understand the anatomy of the heart.
“You can take any anatomical part and show any of it. You can move it around, make it kind of translucent so you can see through the outside, and that really helped me understand like how cardiac anatomy worked,” student Satyam Ghodasara said.
“I actually had a moment where I found the aortic valve and it was the first time I’d actually seen the aortic valve in relation to all the other anatomical structures.
“It was a way of seeing it that you couldn’t do with an actual heart.”
Microsoft is yet to announce when HoloLens will be released and how much it will cost.
But Case Western Reserve University is far from alone in its testing of wearable devices to aid the teaching of medicine.
Last year, surgeons from the University of California, Los Angeles (UCLA) oversaw hernia repair operations by counterparts in Paraguay and Brazil using Google Glass.
The aim is that those trained using Glass would then become trainers for others in their own countries.
UCLA also planned to roll out the program in Haiti, the Dominican Republic, Guatemala and Ecuador.
“We are developing practical applications for these technologies so that surgeons in any setting can have access to the global surgical community from within their own operating rooms,” UCLA’s Dr. Justin Wagner said.
At University of California, San Francisco (UCSF’s) School of Medicine, surgeons use Google Glass to call up “CT scans, MRIs and the like” into their field of vision as they operate on a patient.
Meanwhile, at Ohio State University, Glass was used by surgeons to communicate with people outside the operating theatre.
Closer to home, CSIRO for many years researched the use of haptics – a kind of virtual reality touch technology – for use in surgical training.
“In countries like Australia, where the population is small and unevenly distributed, access to specialist surgical expertise for training can be difficult,” the scientists said.
“Surgical residents commonly travel long distances to attend specialist training courses, at significant expense and disruption to their professional and personal lives.
“[Our] demonstration explores the concept of combining remote interaction with an experienced surgeon instructor and the best attributes of virtual reality technology for this class of training.”
In addition, researchers at Flinders University continue to explore haptics in medical simulators, which are also targeted at training applications.